Lung cancer is the uncontrolled growth of abnormal cells, which may occur in the lining of the trachea, bronchi, bronchioles, or alveoli. Ninety five percent of lung cancers are bronchogenic (arise from the epithelial lining of the bronchial tree).
Cause for Lung Cancers
Carcinogenesis, Initiation by a carcinogen (cancer-causing agent), for example, cigarette smoke, asbestos, or coal dust. Promotion by a secondary factor, for example, number of years smoking or number of cigarettes smoked. Progression, that is, the growth of pre-malignant cells and their ability to metastasize.
Lifestyle risk factors: Smoking, most common risk factor: 85% of people are or were former smokers. Others risk factor is Environmental tobacco smoke (secondhand smoke).About 3,400 lung cancer deaths in nonsmoking adults. Nonsmokers chronically exposed to secondhand smoke may have as much as a 24% increased risk for developing lung cancer.
Occupational risks: Radon, Asbestos fibers e.g. insulation and shipbuilding (7 times increased risk of death in asbestos workers & Asbestos exposure combined with cigarette smoking act synergistically to produce an increased risk of lung cancer), Arsenic (copper refining and pesticides), Beryllium (airline industry and electronics), Metals (nickel or copper), Chromium, Cadmium, Coal tar (mining), Mustard gas, Air pollution: diesel exhaust, Radiation, Tuberculosis.
Biological risks Sex/age: Males have a greater risk of lung cancer than do females, although incidence rate is declining significantly in men, from high of 102 per 100,000 in 1984 to 77.8 per 100,000 in 2002. Lung cancer incidence doubled in females from 1975 to 2000 and now has stabilized. Increased risk is associated with increasing age. 70% of all lung cancers diagnosed in individuals over the age of 65 and the number of cases diagnosed at 50 or earlier is increasing.
Family history: Lung cancer in one parent increases their children’s risk of the diagnosis of lung cancer before age 50.
Genetic predisposition: Genetic susceptibility is a contributing factor in those that develop lung cancer at a younger age. A single gene for lung cancer has not been identified. Abnormalities of p53 gene, a tumor-suppressor gene, have been suggested to be mutated in many people with lung cancer. EGFL6 gene identified as potential tumor marker.
Race: African Americans, native Hawaiians, and non-Hispanic whites have greater risk of lung cancer. Black men between the age of 35 and 64 years of age have twice the risk compared to non-Hispanic Whites.
Chronic inflammation, chronic obstructive pulmonary disease (COPD), and pulmonary fibrosis: Tuberculosis: Scarring of healthy lung tissue may lead to lung cancer development. Pulmonary fibrosis: Silica is the probable lung carcinogen. COPD: Airflow limitation results in a 6.44 times greater risk for lung cancer compared with the risk associated with absence of ventilator impairment.
To categorize lung cancers visible Pathologic features on light microscopy, are used. Lung cancers are divided into two major groups, Small Cell Lung Cancer and Non–Small Cell Lung Cancer
Non-Small Cell Lung Cancer
- Squamous cell (epidermoid forms in the lining of the bronchial tubes). Most common type of lung cancer in men. Decreasing incidence in last two decades. Typically develops in segmental bronchi, causing bronchial obstruction and regional lymph node involvement. Symptoms are related to obstruction : nonproductive cough, pneumonia, atelectasis, that is, a collapsed lung, chest pain is a late symptom associated with bulky tumor, Pancoast Tumor, or pulmonary sulcus tumor, begins in the upper portion of the lung and commonly spreads to the ribs and spine causing classic shoulder pain that radiates down the ulnar nerve distribution. Treatment: surgical resection is preferred before the development of metastatic disease, chemotherapy and radiation therapy to decrease the incidence of recurrence.
- Adenocarcinoma. Most common form in Unites States, Increasing incidence in females. Occurs in non smokers. adenocarcinoma develops in the periphery of the lungs and frequently metastasizes to brain, bone, and liver. Symptoms: no symptoms with small peripheral lesions, Identifi ed by routine chest radiograph/CT scan. Treatment: surgical resection and chemotherapy and radiation therapy to decrease the incidence of recurrence.
- Bronchioalveolar (BAC). Form near the lung’s air sacs. BAC may have abnormal gene in their tumor cells. Targeted chemotherapy treatment appears to be effective.
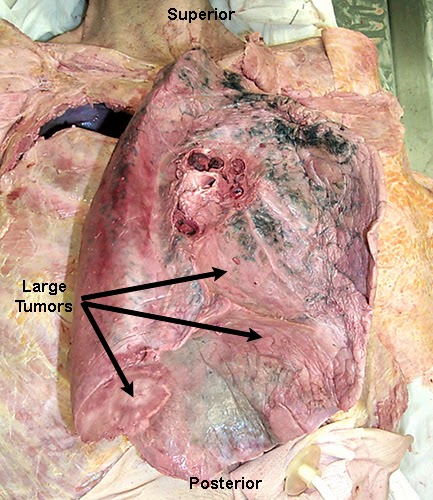
- Large cell. Large cell: 10% of all lung cancer cases. Bulky peripheral tumor. Metastasizing to brain, bone, adrenal glands, or liver. Symptoms related to obstruction or metastatic spread pneumonitis and pleural effusions. Treatment: surgical resection (limited because of the often aggressive course of this tumor type) and chemotherapy and radiation therapy (palliative role to minimize symptoms of advanced disease).
Small-Cell Lung Cancer
Patients with SCLC often have widespread disease at the time of diagnosis. Rapid clinical deterioration in patients with chest masses often indicates SCLC
- Oat cell carcinoma Oat cell carcinoma: 13% of all lung cancers. Most aggressive type, greater tendency to metastasize than Non-Small Cell Lung Cancer Strongly related to cigarette smoking often occurs within the mainstem bronchi and segmental bronchi; 80% of cases have hilar and mediastinal node involvement. Symptoms: Paraneoplastic syndrome: syndrome of inappropriate antidiuretic hormone (SIADH), Hyponatremia, fluid retention, weakness, and fatigue, Ectopic adrenocorticotropic hormone (ACTH) production, Hypokalemia, hyponatremia, hyperglycemia, lethargy, and confusion. Treatment for Oat cell carcinoma, Surgery rarely indicated even in those with limited stage disease because of the need for immediate systemic therapy and chemotherapy and radiation therapy offers the best hope for prolonged survival and quality of life. Majority of the patients respond to chemotherapy and radiation therapy but recurrence rate is very high. Two-thirds of patients demonstrate evidence of extensive disease at the time of diagnosis.
- Non-Bronchogenic Carcinomas. Undifferentiated non-small cell lung cancer (NSCLC). Non-bronchogenic carcinomas undifferientated non-small cell lung cancer (NSCLC) :
Knowing the stage of Lung Cancer is important because treatment is often decided according to the stage of a Lung cancer. TNM staging system. TNM staging takes the following factors into account. The size of the Lung Cancer (T). Whether Lung Cancer cells have spread into the lymph nodes (N) whether the Lung Cancer has spread anywhere else in the body – secondary cancer or metastases (M)
Stage of Lung cancer TNM (Tumor, Nodes, Metastases) system of staging
TNM Stage of Lung cancer Description:
Primary tumor (T)
- TX; Primary tumor cannot be assessed, or tumor proven by the presence of malignant cells in sputum or bronchial washings but not visualized by imaging or bronchoscopy.
- T0 : No evidence of primary tumor
- Tis : Carcinoma in situ
- T1 : Tumor 3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus)
- T2: Tumor with any of the following features of size or extent: 3 cm in greatest dimension. Involves main bronchus, 2 cm distal to the carina Invades the visceral pleura Associated with atelectasis or obstructive pneumonitis that extends to the hilar region but does not involve the entire lung.
- T3 : Tumor of any size that directly invades any of the following: chest wall (including superior sulcus tumors), diaphragm, mediastinum pleura, parietal pericardium; or tumor in the main bronchus, 2 cm distal to the carina, but without involvement of the carina; or associated atelectasis or obstructive pneumonitis of the entire lung
- T4: Tumor of any size that invades any of the following: mediastinum, heart, great vessels, trachea, esophagus, vertebral body, carina; or tumor with a malignant pleural or pericardial effusion, b or with satellite tumor nodule(s) within the ipsilateral primary-tumor lobe of the lung
Regional lymph nodes (N)
- NX Regional lymph nodes cannot be assessed
- N0 No regional lymph node metastasis
- N1 Metastasis to ipsilateral peribronchial and/or ipsilateral hilar lymph nodes, and intrapulmonary nodes involved by direct extension of the primary tumor
- N2 Metastasis to ipsilateral mediastinal and/or subcarinal lymph node(s)
- N3 Metastasis to contralateral mediastinal, contralateral hilar, ipsilateral, or contralateral scalene, or supraclavicular lymph node(s)
Distant Metastasis (M)
- MX Presence of distant metastasis cannot be assessed
- M0 No distant metastasis
- M1 Distant metastasis present
Stage grouping (TNM subsets):
- Stage IA (T1 N0 M0), IB (T2 N0 M0). Most common form of early lung cancer located only in the lungs. Detected on routine chest X-ray in patients who present for unrelated medical condition or routine examination. Treatment-surgical resection.
- Stage IIA (T1 N1 M0), IIB (T2 N1 M0, T3 N0 M0). Tumors in the lung and lymph nodes (hilar and bronchopulmonary nodes). Treatment-surgical resection and adjuvant radiation or chemotherapy, or both. Induction chemotherapy before surgery is being investigated. Patients with significant co-morbid disease surgery may not be an option.
- Stage IIIA (T3 N1 M0, T1 N2 M0, T2 N2 M0, T3 N2 M0) Cancer in the lung and lymph nodes on the same side of the chest. T3 tumors involving the main stem bronchi produce hemoptysis, Dyspnea, wheezing, atelectasis, and post obstructive pneumonia. T3 tumors involving the pericardium or diaphragm may be symptomatic but those involving the chest wall usually cause pain. Nodal disease is often asymptomatic, if extensive nodal disease may cause compression of the proximal airways and superior vena cava syndrome. Treatment—selected cases surgical resection (T3NO-1), commonly multi-modality therapy with chemotherapy being primary form of treatment; multiple trials of combined chemotherapy, radiation with or without surgery are under investigation.
Stage
- IIIB (T4 N0 M0, T4 N1 M0, T4 N2 M0, T1 N3 M0, T2 N3 M0, T3 N3 M0, T4 N3 M0) Cancer has spread to the lymph nodes on the opposite side of the chest. T4 tumors invade the mediastinum structures, and/or malignant pleural effusions. N3—metastases. Treatment—chemotherapy and radiation therapy; in rare exceptions, surgery may be considered.
- Stage IV (Any T Any N M1) Evidence of metastatic disease. Treatment often palliative (to relieve symptoms). Clinical trials may offer some survival benefit.
Like many other neoplasm disease Complications of Lung Cancer occurs when lung cancer metastasized to other organ, outside the Lung. Disease progression and metastasis cause various complications. Early stage and localized disease may be asymptomatic. Symptoms are often medically treated and attributed to conditions such as bronchitis, pneumonia, and chronic obstructive pulmonary disease. Symptoms: cough & wheezing, increased sputum production, hemoptysis, Dyspnea, pneumonia, pleural effusions.
Advanced disease predominant at time of diagnosis related to tumor growth and compression of adjacent structures. When the primary tumor spreads to intrathoracic structures, complications may include tracheal obstruction; esophageal compression with dysphagia; phrenic nerve paralysis with hemidiaphragm elevation and dyspnea; sympathetic nerve paralysis with Horner’s syndrome with ptosis, miosis, hemifacial anhydrosis, clubbing, hypertrophic osteoarthropathy, bone pain, fatigue, dysphagia from esophageal compression, wheezing or stridor, phrenic nerve paralysis with elevated hemidiaphragm, arrhythmias and heart failure (from pericardial involvement), hypoxia related to lymphangitic spread, superior vena cava syndrome (swelling of the face, neck and upper extremities and related to compression of blood vessels in the neck and upper thorax.
Symptoms: chronic cough, Dyspnea, weight loss, increased sputum production, hemoptysis, hoarseness (involvement of the laryngeal nerve), pleural effusions and atelectasis, chronic pain, pain over the shoulder and medial scapula, arm pain with or without muscle wasting along ulnar distribution,
Lung cancer usually cause breathing and heart problems such as:
- Pleural effusion
- Pericardial effusion
- Coughing up large amounts of bloody sputum.
- Collapse of a lung (pneumothorax).
- Blockage of the airway (bronchial obstruction).
- Recurrent infections, such as pneumonia.
Other complications are anorexia and weight loss, sometimes leading to cachexia, digital clubbing, and hypertrophic osteoarthropathy. Endocrine syndromes may involve production of hormones and hormone precursors.
Extra thoracic spread of disease: adrenal glands (50%), liver (30%), brain (20%), bone (20%), kidneys (15%), scalene lymph nodes. Prognosis remains poor and has improved very slightly despite medical advances: <14% combined 5-year survival rate
A common treatment method of Lung Cancer is Surgery, chemotherapy and radiotherapy is all classified as a treatment for lung cancer. Knowing the stage of Lung Cancer is important because treatment is often decided according to the stage of a Lung cancer. Lung cancer accounts for more deaths than prostate, breast, and colon cancer combined. The 1-year survival rate remains approximately 41%, and the 5-year survival rate is 15%. Only 16% of lung cancers are found at an early, localized stage, when the 5-year survival rate is 49%. The survival rate for lung cancer has not improved over the last 10 years.
Common treatment methods of Lung Cancer:
Surgery Treatment for Lung Cancer
The treatment of choice for non-small cell lung cancer, Stage IA, IB, IIA, IIB, and selected cases of stage IIIA : lobectomy (removal of a lobe of the lung), pneumonectomy (removal of one lung), wedge resection or segmentectomy for patients with inadequate pulmonary reserve who cannot tolerate lobectomy, VATS (Video Assisted Thoroscopic Surgery), palliative surgery. Before surgery patient must know the risk factor from Lung Cancer Surgery; Risks from lung cancer surgery include damage to structures in or near the lungs, general risks related to surgery, and risks from general anesthesia
Patient education before surgery: patient understands surgical procedure, incision, placement of chest tubes; smoking cessation before surgery to reduce pulmonary complications pain control; bronchodilators, coughing and deep-breathing exercises, early ambulation after surgery.
After surgery : assess respiratory function (respiratory rate, level of dyspnea, use of accessory muscles, and arterial blood gases); monitor chest tube drainage and air leaks, monitor oxygen saturation at rest and ambulation, assess pain control, chest physical therapy (bronchial drainage positions, deep breathing, coughing) early ambulation,monitor for atrial arrhythmias ; discharge planning and home care arrangements.
Chemotherapy Treatment for Lung Cancer
Researchers are continually looking at different ways of combining new and old drugs for advanced non-small cell lung cancer.
Chemotherapy Treatment for Non-Small Cell Lung Cancer
- Customize treatment: Erlotinib (Tarceva) for people whose tumors have epidermal growth factor receptors, a genetic mutation. Gefitinib (Iressa) effective in people whose lung tumors have similar genetic mutations.
- Targeted treatments for advanced non-small cell lung cancer; Sunitinib (Sutent) works by cutting off blood supply and blockingnthe cancer cells their ability to grow. Sorafenib (Nexavar) suppresses receptors for vascular endothelial growth factor platelet derived growth factor—plays a critical role in the growth of blood vessels that feed the cancer (angiogensis).
- Combined methods are the treatment of choice for selected cases of stage IIIA and IIIB; Cispatin, Paclitaxel and Gemcitabine, Gemcitabine and Vinorelbine, Carboplatin and Paclitaxel and radiation, Cisplatin and Vinblastine and radiation
- Stage IV; Carboplatin and Paclitaxel, Carboplatin and Gemcitabine, Cisplatin and Vinorelbine, Docetaxel and Gemcitabine, Pemetrexed, Chemotherapy combined with Cetuximab (Erbitux): Cetuximab binds to epidermal growth factor receptors (EGFR), preventing a series of reactions in the cell that lead to lung cancer.
- Progression of disease: Single-agent Docetaxel, Gemcitabine, Paclitaxel
- Investigational New treatment approaches are being investigated all the time. Mage-A3 vaccine and non-small cell lung cancer, Bortezomib (Velcade) proteasome inhibitors destroys cancer cells
Chemotherapy Treatment for Small-Cell Lung Cancer
- Limited-stage disease; Pulmonary resection stage I or stage II, Etoposide and Cisplatin and Radiation, Etoposide and Carboplatin
- Extensive stage disease: Etoposide and Carboplatin +/− Paclitaxel, Adriamycin, Cyclophosphamide
- Investigational: Vaccine-autologous dendritic cell-adenovirus p53
Chemotherapy treatment Complications, Myelosuppression (infection, anemia, bleeding), nephrotoxicity, nausea and vomiting, mucositis (inflammation of the mucous membranes), fatigue, SIADH and hyponatremia, hypotension, anaphylaxis, alopecia (hair loss), neurotoxicity (peripheral neuropathies, central nervous system toxicity), cardiomyopathy, arrhythmias, congestive heart failure, myocardial infarction, pneumonitis or pulmonary fibrosis, taste changes.
Patient education (chemotherapy): chemotherapeutic agents, treatment schedule, adverse effects of drugs.
Radiation therapy Treatment for Lung Cancer
- External beam radiotherapy used as an adjunct to surgery to decrease tumor size, to cure patients considered inoperable for medical or pathologic reasons, or to decrease symptoms. Radiation after surgery: to improve resectability of tumor & to sterilize microscopic disease. Radiation after surgery: to treat disease confined to one hemi thorax with hilar or mediastinum nodal metastasis & to reduce local recurrence (if positive surgical margins exist). Prophylactic cranial irradiation: limited disease small-cell lung cancer to reduce reoccurrence in CNS.
- Brachytherapy placement of radioactive sources (seeds or catheter) directly into or adjacent to a tumor. Intraoperative: reduce local recurrence. Symptom palliation (relief of pain from bone metastases, hemoptysis, superior vena cave syndrome, airway obstruction).
Complications of radiation therapy: Dyspnea, cough, initial increase in mucus production, and then dry cough, fatigue, skin erythema, esophagitis and dysphagia, pneumonitis, lung fibrosis.
Patient education: radiation therapy: indelible markings, treatment schedule, site-specific adverse effects (within treatment field).
Treatment alternatives
Neoadjuvant is therapy given before the primary therapy to improve effectiveness (e.g., chemotherapy or radiation before surgery). Adjuvant treatments are equally beneficial and often given concurrently or immediately following one another to maximize effectiveness (e.g., surgery and adjuvant chemotherapy after surgery), multimodality is therapy that combines more than one method of treatment (e.g. concurrent chemotherapy and radiation, such as, adjuvant and Neoadjuvant)
Home care considerations
After lung surgery: smoking cessation, control of incision pain, wound care, breathing exercises and coughing, pursed lip breathing exercises, maintain fluid intake, maintaining your nutrition, resume activity, regaining arm and shoulder function.
During and after radiation therapy: monitor side effects of radiation therapy and report any change in.
Symptoms: Dyspnea, fatigue is common lasting 4–6 weeks after therapy, good nutrition, liquid diet supplement during periods of esophagitis, avoid wearing tight clothes, skin care.
During and after chemotherapy, advise patients:
To identify all treatment related side effects and report changes
Fatigue may last weeks to months
To plan their day, and allow for periods of rest
Try activities such as yoga, exercise, meditation, and guided imagery
Keep a diary and document symptoms, activity level, nutrition, treatments, and emotions
To monitor effectiveness of pain medications
To monitor for any signs of infection, such as an increased temperature, redness or swelling, and that the latter symptoms may not be present during weeks of impaired immunity following chemotherapy administration
Monitor weight change and appetite
Nutritional supplements
Pulmonary rehabilitation programs: exercise strengthening, breathing exercises, walking program, nebulizers/aerosol medication delivery, disease specific instruction and support. Support groups: Lung Cancer specific, Better Breathers Club a support group sponsored by the American Lung Association for patients with chronic lung disease. Hospice: dignified dying, pain management, end of life issues, patient/family support.
Nursing Assessment
Patient History
Establish a history of persistent cough, chest pain, Dyspnea, weight loss, or hemoptysis. Smoking history, other risk factors (family history, occupational risks), associated diseases (COPD, tuberculosis, and emphysema), symptom description and onset. Ask if the patient has experienced a change in normal respiratory patterns or hoarseness. Some patients initially report pneumonia, bronchitis, and epigastria pain, symptoms of brain metastasis, arm or shoulder pain, or swelling of the upper body. Ask if the sputum has changed color, especially to a bloody, rusty, or purulent hue. Elicit a history of exposure to risk factors by determining if the patient has been exposed to industrial or air pollutants. Check the patient’s family history for incidence of lung cancer
Physical examination
The clinical findings of lung cancer may be localized to the lung or may result from the regional or distant spread of the disease. Lung auscultation, respiratory rate and depth, palpitation of supraclavicular area for tumor or lymphatic involvement or both, clubbing, nicotine stains to skin, hair, teeth. Lung cancer clinical manifestations depend on the type and location of the tumor. Because the early stages of this disease usually produce no symptoms, it is most often diagnosed when the disease is at an advanced stage. In 10% to 20% of patients, lung cancer is diagnosed without any symptoms, usually from an abnormal finding on a routine chest x-ray.
Auscultation may reveal a wheeze if partial bronchial obstruction has occurred. Auscultate for decreased breath sounds, rales, or rhonchi. Note signs of an airway obstruction, such as extreme shortness of breath, the use of accessory muscles, abnormal retractions, and stridor. Monitor the patient for oxygenation problems, such as increased heart rate, decreased blood pressure, or an increased duskiness of the oral mucous membranes. Metastases to the mediastinum lymph nodes may involve the laryngeal nerve and may lead to hoarseness and vocal cord paralysis. The superior vena cava may become occluded with enlarged lymph nodes and cause superior vena cava syndrome; note edema of the face, neck, upper extremities, and thorax.
Psychosocial examination
The patient is faced with a psychological adjustment to the diagnosis of a chronic illness that frequently results in death. Patient undergoes major lifestyle changes as a result of the physical side effects of cancer and its treatment. Interpersonal, social, and work role relationships change. Evaluate the patient for evidence of altered moods such as depression or anxiety, and assess the patient’s coping mechanisms and support system.
Diagnostic tests For Lung Cancer
Chest radiographs plain anterior-posterior and lateral views not reliable to find lung tumors in their earliest stage.
Chest Computed Tomography (CT) three-dimensional image of the lungs and lymph nodes (can detect tumors as small as 5 millimeters). CT is only about 80% accurate in predicting mediastinum node involvement.
Spiral computed tomography of the chest.
Magnetic Resonance Imaging (MRI) 92% accuracy in the diagnosis of mediastinum invasion.
Positron Emission Tomography (PET) scan is based upon increased glucose metabolism in cancer cells. The PET scan uses a glucose analogue radiopharmaceutical to identify increased glycolysis in tumor tissues. The PET scan is a highly sensitive test in the diagnosis and staging of lung cancer.
Bronchoscopic detection of tumor auto fluorescence could improve cure rates in selected groups at high-risk.
Sputum cytology
Percutaneous transthoracic needle biopsy
Fine needle aspiration or biopsy
Bronchoscopy.
Mediastinoscopy to evaluate lymph node involvement.
Scalene node biopsy (evaluate lymph node involvement)
Photodynamic therapy; An injection of a light-sensitive agent with uptake by cancer cells, followed by exposure to a laser light within 24 to 48 hours, will result in fluorescence of cancer cells or cell death. Especially helpful in identifying developing cancer cells or “carcinoma in-situ.” Also used to determine the extent of disease and the response to treatment (experimental).
Assessment of distant metastasis: Abdominal CT (identify adrenal or liver metastasis), Head CT, MRI (brain), Bone scan; Thoracentesis (detect malignant cells in the pleural fluid).
Nursing Diagnosis for Lung Cancer
Common Nursing diagnosis found in nursing care plans for patient with Lung Cancer:
Impaired gas exchange related to Removal of lung tissue, altered oxygen supply.
Ineffective Airway Clearance May be related to Increased amount or viscosity of secretions, Restricted chest movement, pain, Fatigue, weakness
Acute Pain May be related to Surgical incision, tissue trauma, and disruption of intercostals nerves, Presence of chest tube, Cancer invasion of pleura, chest wall
Fear/Anxiety [specify level] May be related to Situational crises, Threat to or change in health status, Perceived threat of death.
Deficient Knowledge [Learning Need] regarding condition, treatment, prognosis, self-care, and discharge needs. May be related to Lack of exposure, unfamiliarity with information or resources, Information misinterpretation, Lack of recall
Sample Nursing care Plan for Lung Cancer with interventions and rationale
Impaired gas exchange
May be related to:
- Removal of lung tissue (Surgery Treatment for Lung Cancer)
- Altered oxygen supply hypoventilation
- Decreased oxygen-carrying capacity of blood (blood loss).
Nursing outcomes and evaluation criteria client will:
Respiratory status: gas exchange, Demonstrate improved ventilation and adequate oxygenation of tissues by arterial blood gases (ABGs) within client normal range, be free of symptoms of respiratory distress, the patient will maintain adequate ventilation. The patient will maintain a patent airway.
Nursing Interventions Nursing care Plan for Lung Cancer Nursing diagnosis Impaired gas exchange:
Respiratory Management:
Note respiratory rate, depth, and ease of respirations. Observe for use of accessory muscles, pursed-lip breathing, or changes in skin or mucous membrane Rationale Respirations may be increased as a result of compensatory mechanism to accommodate for loss of lung tissue or pain.
Auscultate lungs for air movement and abnormal breath sounds. Rationale Consolidation and lack of air movement on operative side are normal in the client who has had a pneumonectomy; but in a client who has had a lobectomy should demonstrate normal airflow in remaining lobes.
Investigate restlessness and changes in mentation and level of consciousness. Rationale May indicate increased hypoxia or complications such as mediastinum shift in a client who has had a pneumonectomy when accompanied by tachypnea, tachycardia, and tracheal deviation.
Assess client response to activity. Encourage rest periods, limiting activities to client tolerance. Rationale Increased oxygen consumption and demand and stress of surgery may result in increased Dyspnea and changes in vital signs with activity; however, early mobilization is desired to help prevent pulmonary complications and to obtain and maintain respiratory and circulatory efficiency. Adequate rest balanced with activity can prevent respiratory compromise.
Note development of fever. Rationale Fever within the first 24 hours after surgery is frequently due to atelectasis. Temperature elevation within postoperative day 5 to 10 usually indicates an infection, such as wound or systemic.
Airway Management:
Maintain patent airway by positioning, suctioning, and use of airway adjuncts. Rationale Airway obstruction impedes ventilation, impairing gas exchange. (Refer to ND: ineffective Airway Clearance).
Reposition frequently, placing client in sitting and supine to side positions. Rationale Maximizes lung expansion and drainage of secretions.
Avoid positioning client with a pneumonectomy on the operative side. Rationale Research shows that positioning clients following lung surgery with their “good lung down” maximizes oxygenation by using gravity to enhance blood flow to the healthy lung, thus creating the best possible match between ventilation and perfusion.
Encourage and assist with deep-breathing exercises and pursed lip breathing, as appropriate. Rationale Promotes maximal ventilation and oxygenation and reduces or prevents atelectasis.
Administer supplemental oxygen via nasal cannula, partial rebreathing mask, or high-humidity face mask, as indicated. Rationale Maximizes available oxygen, especially while ventilation is reduced because of anesthetic, depression, or pain, and during period of compensatory physiological shift of circulation to remaining functional alveolar units.
Assist with and encourage use of incentive spirometer. Rationale Prevents or reduces atelectasis and promotes reexpansion of small airways.
Monitor and graph ABGs and pulse oximetry readings. Note hemoglobin (Hgb) levels. Rationale Decreasing PaO2 or increasing PaCO2 may indicate need for ventilatory support. Significant blood loss results in decreased oxygen-carrying capacity, reducing PaO2.
Tube Care Chest:
Maintain patency of chest drainage system following lobectomy and segmental wedge resection procedures. Rationale Drains fluid from pleural cavity to promote re expansion of remaining lung segments.
Note changes in amount or type of chest tube drainage. Rationale Bloody drainage should decrease in amount and change to a more serous composition as recovery progresses. A sudden increase in amount of bloody drainage or return to frank bleeding suggests thoracic bleeding or a hemothorax, sudden cessation suggests blockage of tube, requiring further evaluation and intervention.
Observe for presence of bubbling in water-seal chamber. Rationale Air leaks appearing immediately postoperatively are not uncommon, especially following lobectomy or segmental resection; however, this should diminish as healing progresses. Prolonged or new leaks require evaluation to identify problems in client versus a problem in the drainage system.
Nursing diagnosis Ineffective Airway Clearance
May be related to:
- Increased amount or viscosity of secretions
- Restricted chest movement, pain
- Fatigue, weakness
Nursing Outcomes and Evaluation Criteria Client Will:
- Respiratory Status: Airway Patency
- Demonstrate patent airway, with fluid secretions easily expectorated, clear breath sounds, and noiseless respirations.
Nursing Interventions nursing care Plan for Lung Cancer Nursing diagnosis Ineffective Airway Clearance
- Auscultate chest for character of breath sounds and presence of secretions. Rationale: Noisy respirations, rhonchi, and wheezes are indicative of retained secretions or airway obstruction.
- Assist client with and provide instruction in effective deep breathing, coughing in upright position (sitting), and splinting of incision. Rationale Upright position favors maximal lung expansion, and splinting improves force of cough effort to mobilize and remove secretions. Splinting may be done by nurse placing hands anteriorly and posterior over chest wall and by client, with pillows, as strength improves.
- Observe amount and character of sputum and aspirated secretions. Investigate changes, as indicated. Rationale Increased amounts of colorless (or blood-streaked) or watery secretions are normal initially and should decrease as recovery progresses. Presence of thick, tenacious, bloody, or purulent sputum suggests development of secondary problems for example, dehydration, pulmonary edema, local hemorrhage, or infection that require correction or treatment.
- Suction if cough is weak or breathe sounds not cleared by cough effort. Avoid deep endotracheal and nasotracheal suctioning in client who has had pneumonectomy if possible. Rationale Suctioning increases risk of hypoxemia and mucosal damage. Deep tracheal suctioning is generally contraindicated. If suctioning is unavoidable, it should be done gently and only to induce effective coughing.
- Encourage oral fluid intake, within cardiac tolerance. Rationale Adequate hydration aids in keeping secretions loose and enhances expectoration.
- Assess for pain and discomfort and medicate on a routine basis and before breathing exercises. Rationale Encourages client to move, cough more effectively, and breathe more deeply to prevent respiratory insufficiency.
- Provide and assist client with incentive spirometer and postural drainage and percussion, as indicated. Rationale Improves lung expansion and ventilation and facilitates removal of secretions. Note: Postural drainage may be contraindicated in some clients, and, in any event, must be performed cautiously to prevent respiratory embarrassment and incision discomfort.
- Use humidified oxygen and ultrasonic nebulizer. Provide additional fluids intravenously (IV), as indicated. Rationale Maximal hydration helps promote expectoration. Impaired oral intake necessitates IV supplementation to maintain hydration.
- Administer bronchodilators, expectorants, and analgesics, as indicated. Rationale Relieves bronchospasm to improve airflow. Expectorants increase mucus production and liquefy and reduce viscosity facilitating removal of secretions.
Nursing Diagnosis Acute Pain
May be related to:
- Surgical incision, tissue trauma, and disruption of intercostals nerves
- Presence of chest tubes
- Cancer invasion to pleura or chest wall
Nursing Outcomes and Evaluation Criteria Client Will:
- Pain Level
- Report pain relieved or controlled.
- The patient will express feelings of comfort and decreased pain
- Appear relaxed and sleep or rest appropriately.
- Participate in desired as well as needed activities.
Nursing Interventions and rationale nursing care Plan for Lung Cancer with nursing diagnosis Acute Pain
- Ask client about pain. Determine pain location and characteristics. Have client rate intensity on a scale of 0 to 10. Rationale Helpful in evaluating cancer related pain symptoms, which may involve viscera, nerve, or bone tissue. Use of rating scale aids client in assessing level of pain and provides tool for evaluating effectiveness of analgesics, enhancing client control of pain.
- Assess client verbal and nonverbal pain cues. Rationale Discrepancy between verbal and nonverbal cues may provide clues to degree of pain and need for and effectiveness of interventions.
- Note possible pathophysiological and psychological causes of pain. Rationale Fear, distress, anxiety, and grief can impair ability to cope. Posterolateral incision is more uncomfortable for client than an anterolateral incision. Discomfort can greatly increase with the presence of chest tubes.
- Evaluate effectiveness of pain control. Encourage sufficient medication to manage pain; change medication or time span as appropriate. Rationale Pain perception and pain relief are subjective, thus pain management is best left to client’s discretion. If client is unable to provide input, the nurse should observe physiological and nonverbal signs of pain and administer medications on a regular basis.
- Encourage verbalization of feelings about the pain. Rationale Fears and concerns can increase muscle tension and lower threshold of pain perception.
- Provide comfort measures such as frequent changes of position, back rubs, and support with pillows. Encourage use of relaxation techniques including visualization, guided imagery, and appropriate Diversional activities. Rationale Promotes relaxation and redirects attention. Relieves discomfort and therapeutic effects of analgesia.
- Schedule rest periods, provide quiet environment. Rationale Decreases fatigue and conserves energy, enhancing coping abilities.
- Assist with self care activities, breathing, arm exercises, and ambulation. Rationale Prevents undue fatigue and incision strain. Encouragement and physical assistance and support may be needed for some time before client is able or confident enough to perform these activities because of pain or fear of pain.
- Assist with patient-controlled analgesia PCA or analgesia through epidural catheter. Administer intermittent analgesics routinely, as indicated, especially 45 to 60 minutes before respiratory treatments, and deep-breathing and coughing exercises. Rationale Maintaining a constant drug level avoids cyclic periods of pain, aids in muscle healing, and improves respiratory function and emotional comfort and coping.
Nursing Diagnosis Fear/Anxiety [specify level]
May be related to:
- Situational crises
- Threat to or change in health status
- Perceived threat of death
Nursing Outcomes and Evaluation Criteria Client Will:
- Fear Self-Control or Anxiety Self-Control
- Acknowledge and discuss fears and concerns.
- Demonstrate appropriate range of feelings and appear relaxed and resting appropriately.
- Verbalize accurate knowledge of situation.
- Report beginning use of individually appropriate coping strategies.
Nursing Interventions and rationale nursing care Plan for Lung Cancer with nursing diagnosis Fear/Anxiety:
- Evaluate client and significant other (SO) level of understanding of diagnosis. Rationale Client and SO are hearing and assimilating new information that includes changes in self-image and lifestyle. Understanding perceptions of those involved sets the tone for individualizing care and provides information necessary for choosing appropriate interventions.
- Acknowledge reality of client’s fears and concerns and encourage expression of feelings. Rationale Support may enable client to begin exploring and dealing with the reality of cancer and its treatment. Client may need time to identify feelings and even more time to begin to express them.
- Provide opportunity for questions and answer them honestly. Be sure that client and care providers have the same understanding of terms used. Rationale Establishes trust and reduces misperceptions or misinterpretation of information.
- Accept, but do not reinforce, client’s denial of the situation. Rationale When extreme denial or anxiety is interfering with progress of recovery, the issues facing client need to be explained and resolutions explored.
- Note comments and behaviors indicative of beginning acceptance or use of effective strategies to deal with situation. Rationale Fear and anxiety will diminish as client begins to accept and deal positively with reality. Indicator of client’s readiness to accept responsibility for participation in recovery and to “resume life.”
- Involve client and SO in care planning. Provide time to prepare for events and treatments. Rationale May help restore some feeling of control and independence to client who feels powerless in dealing with diagnosis and treatment.
- Provide for client’s physical comfort. Rationale It is difficult to deal with emotional issues when experiencing extreme or persistent physical discomfort.
Nursing Diagnosis Deficient Knowledge Learning Need regarding condition, treatment, prognosis, self-care, and discharge needs
Related to:
- Lack of exposure, unfamiliarity with information or resources
- Information misinterpretation
- Lack of recall
Nursing Outcomes and Evaluation Criteria Disease Process and Treatment Regimen Client Will:
- Verbalize understanding of ramifications of diagnosis, prognosis, and possible complications.
- Participate in learning process Knowledge of the Disease Process.
- Verbalize understanding of therapeutic regimen.
- Correctly perform necessary procedures and explain reasons for the actions.
- Initiate necessary lifestyle changes.
Nursing Interventions and rationale nursing care Plan for Lung Cancer with nursing diagnosis Deficient Knowledge Learning Need regarding condition, treatment, prognosis, self-care, and discharge needs:
- Discuss diagnosis, current and planned therapies, and expected outcomes. Rationale Provides individually specific information, creating knowledge base for subsequent learning regarding home management. Radiation or chemotherapy may follow surgical intervention, and information is essential to enable the client and SO to make informed decisions.
- Reinforce surgeon’s explanation of particular surgical procedure, providing diagram as appropriate. Incorporate this information into discussion about short- and long-term recovery expectations. Rationale Length of rehabilitation and prognosis depend on type of surgical procedure, preoperative physical condition, and duration and degree of complications.
- Discuss necessity of planning for follow-up care before discharge. Rationale Follow-up assessment of respiratory status and general health is imperative to assure optimal recovery. Also provides opportunity to readdress concerns or questions at a less stressful time.
- Identify signs and symptoms requiring medical evaluations, such as changes in appearance of incision, development of respiratory difficulty, fever, increased chest pain, and changes in appearance of sputum. Rationale Early detection and timely intervention may prevent or minimize complications. Stress importance of avoiding exposure to smoke, air pollution, and contact with individuals with upper respiratory infections (URIs).
- Review nutritional and fluid needs. Suggest increasing protein and use of high-calorie snacks as appropriate. Rationale Meeting cellular energy requirements and maintaining good circulating volume for tissue perfusion facilitate tissue regeneration and healing process.
- Identify individually appropriate community resources, such as American Cancer Society, visiting nurse, social services, and home care. Rationale Agencies such as these offer a broad range of services that can be tailored to provide support and meet individual needs.
- Help client determine activity tolerance and set goals. Rationale Weakness and fatigue should decrease as lung heals and respiratory function improves during recovery period, especially if cancer was completely removed. If cancer is advanced, it is emotionally helpful for client to be able to set realistic activity goals to achieve optimal independence.
- Evaluate availability and adequacy of support system(s) and necessity for assistance in self-care and home management. Rationale General Weakness and activity limitations may reduce individual’s ability to meet own needs.
- Encourage alternating rest periods with activity and light tasks with heavy tasks. Stress avoidance of heavy lifting and isometric or strenuous upper body exercise. Reinforce physician’s time limitations about lifting. Rationale Generalized weakness and fatigue are usual in the early recovery period but should diminish as respiratory function improves and healing progresses. Rest and sleep enhance coping abilities, reduce nervousness (common in this phase), and promote healing. Note: Strenuous use of arms can place undue stress on incision because chest muscles may be weaker than normal for 3 to 6 months following surgery.
- Recommend stopping any activity that causes undue fatigue or increased shortness of breath. Rationale Exhaustion aggravates respiratory insufficiency.
- Instruct and provide rationale for arm and shoulder exercises. Have client or SO demonstrate exercises. Encourage following graded increase in number and intensity of routine repetitions. Rationale Simple arm circles and lifting arms over the head or out to the affected side are initiated on the first or second postoperative day to restore normal range of motion ROM of shoulder and to prevent ankylosis of the affected shoulder.
- Encourage inspection of incisions. Review expectations for healing with client. Rationale Healing begins immediately, but complete healing takes time. As healing progresses, incision lines may appear dry with crusty scabs. Underlying tissue may look bruised and feel tense, warm, and lumpy (resolving hematoma).
- Instruct client and SO to watch for and report places in incision that do not heal or reopening of healed incision, any drainage (bloody or purulent), and localized area of swelling with redness or increased pain that is hot to touch. Rationale Signs and symptoms indicating failure to heal, development of complications requiring further medical evaluation and intervention.
- Suggest wearing soft cotton shirts and loose fitting clothing, cover portion of incision with pad, as indicated, and leave incision open to air as much as possible. Rationale Reduces suture line irritation and pressure from clothing. Leaving incisions open to air promotes healing process and may reduce risk of infection.
- Shower in warm water, washing incision gently. Avoid tub baths until approved by physician. Rationale Keeps incision clean and promotes circulation and healing.
- Support incision with butterfly bandages as needed when sutures and staples are removed. Rationale Aids in maintaining approximation of wound edges to promote healing.
Patient Teaching, Discharge And Home Healthcare Guidelines
Patient Teaching, Discharge and Home Healthcare Guidelines for patient with Lung Cancer usually divide in to before surgery and post surgery. Be sure the patient understands any medication prescribed, including dosage, route, action, and side effects. Teach the patient about medical procedure before surgery and post surgery. Teach the patient how to maximize her or his respiratory effort.
Before surgery, supplement and reinforce what the physician has told the patient about the disease and the operation.
Teach the patient about postoperative procedures and equipment. Discuss urinary catheterization, chest tubes, endotracheal tubes, dressing changes, and I.V. therapy.
If the patient is receiving chemotherapy or radiation therapy, explain possible adverse effects of these treatments. Teach him ways to avoid complications, such as infection. Also review reportable adverse effects.
Educate high-risk patients about ways to reduce their chances of developing lung cancer or recurrent cancer.
Refer smokers to local branches of the American Cancer Society or Smokenders. Provide information about group therapy, individual counseling, and hypnosis.
Urge all heavy smokers older than age 40 to have a chest X-ray annually and cytologic sputum analysis every 6 months. Also encourage patients who have recurring or chronic respiratory tract infections, chronic lung disease, or a nagging or changing cough to seek prompt medical evaluation.
Post Surgery, Provide the patient with the names, addresses, and phone numbers of support groups, such as the American Cancer Society, the National Cancer Institute, the local hospice, the Alliance for Lung Cancer Advocacy, Support & Education (ALCASE), and the Visiting Nurses Association
Teach the patient to recognize the signs and symptoms of infection at the incision site, including redness, warmth, swelling, and drainage. Explain the need to contact the physician immediately
Warn an outpatient to avoid tight clothing, sunburn, and harsh ointments on his chest. Teach him exercises to prevent shoulder stiffness.
Teach him how to cough and breathe deeply from the diaphragm and how to perform range-of-motion exercises. Reassure him that analgesics and proper positioning will help to control postoperative pain.